We provide diagnosis, treatment, and management of diseases which affect the human eye and visual system. Some examples include:
Ocular Disease
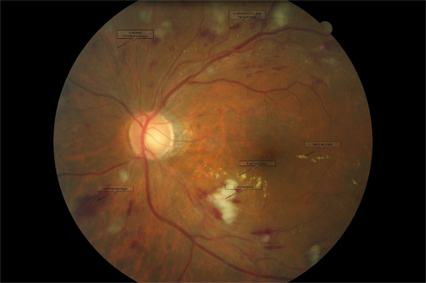 Diabetic Retinopathy
Diabetic Retinopathy
Is a condition associated with diabetes that leads to damage to the retina, the sensitive nerve tissue responsible for sensing light and forming images that we see. When a diabetic person’s blood sugar gets too high, it starts a series of events which causes damage to blood vessel walls. These damaged blood vessels begin to leak blood and fluid into the retina. This results in loss of oxygen and swelling of the retina which causes vision loss over time. The longer one has diabetes and the worse the control of one’s blood sugar levels, the greater the risk of diabetic retinopathy and vision loss related to the disease. Preventative care is key to preserving vision loss from diabetic retinopathy, the leading cause of blindness in the United States. Annual dilated eye exams are recommended for all diabetic patients. Our office has sophisticated technology that our doctors rely on to evaluate the current health & function of your eyes. This includes digital retinal imaging (photographs) of your retina, optical coherence tomography (OCT) which provides a cross-sectional view of the retina (similar to an MRI) and electroretinography (ERG) which evaluates the function of your retinal cells (similar to an EKG to evaluate heart function). Our doctors will evaluate the health of your eye and discuss ways you may be able to protect your eyesight including tight blood sugar control, regular checkups and specific eye vitamins to promote eye health.
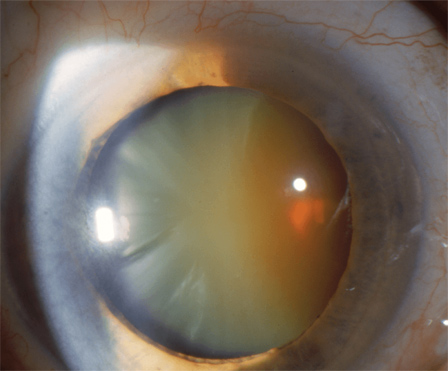 Cataract
Cataract
Is a clouding of the natural internal lens of the eye. The lens is responsible for filtering and focusing incoming light into the eye onto your retina. When a cataract forms, entering light becomes scattered, causing images to appear hazy, shadowed or blurred. It may cause difficulties with night driving, reading, or performing other daily tasks. You may find you need more light to read, especially fine print or poor contrast materials. Sometimes, changes in your glasses prescription may improve vision affected by cataracts. However, once a cataract becomes too advanced and cloudy, surgical intervention is usually the best option to improve your quality of vision when “stronger glasses” no longer provides adequate function. While cataracts are a normal consequence of the aging process, certain risk factors may accelerate cataract formation including: diabetes, steroid use, trauma, UV exposure, smoking, family history and poor diet. Talk to our doctors about whether you may have the onset of cataracts, and how we may be able to improve your vision with a new prescription or if it may be time to consider surgery.
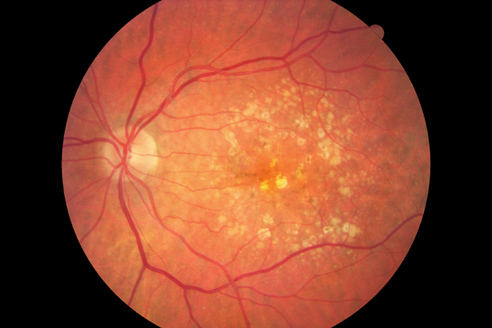 Macular Degeneration
Macular Degeneration
Is an age-related condition in which the central part of the back of the eye (the retina) breaks down and causes central vision loss. This may affect one’s ability to read, drive or recognize faces as portions of the central vision gradually become blurred, distorted, or missing over time. There are two forms of macular degeneration: dry and wet. Dry macular degeneration tends to cause slow progressive loss of vision over time. Wet (or Exudative) macular degeneration tends to cause more rapid vision loss, sometimes in matter of weeks or months. However, both can cause permanent and devastating vision loss. Early detection and treatment can slow the progression of macular degeneration and preserve vision. Risk factors for macular degeneration include: age (over 50), family history, gender (female>male), lighter skin/eye color, history of smoking, poor diet, obesity and low macular pigment. Talk to our doctors about how we may be able to screen for these risk factors and discuss the best options for prevention and treatment of macular degeneration.
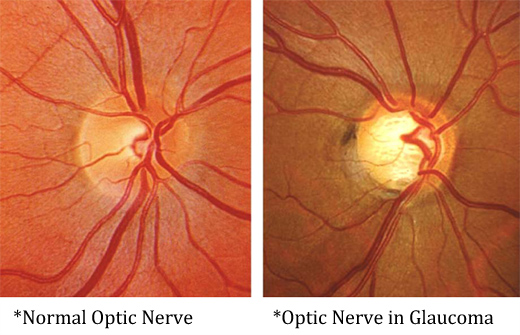 Glaucoma
Glaucoma
Is a disease that involves the deterioration of the optic nerve (responsible for sending images formed by the retina back to the brain to be interpreted). Glaucoma causes slow irreversible loss of vision that is not detectable to the patient until the very end stage. Fortunately, damage from glaucoma is largely preventable with early diagnosis and treatment. Sophisticated technology in our office including: digital retinal photography (monitors changes in the appearance of the optic nerve over time), Humphrey Visual Field Analyzer (assesses the nerve’s responsiveness to light and monitors change from baseline), and Zeiss Optical Coherence Tomographer (provides age related normative data to assess if a nerve is normal or suspicious for glaucoma AND measures microscopic changes in the tissue of the optic nerve over time) allows us to detect early damage and progression related to glaucoma. The information obtained from this technology helps determine if initiating treatment is warranted in the case of a “glaucoma suspect” (someone with multiple risk factors and early warning signs), or if a confirmed glaucoma patient requires a change in their treatment plan. There are multiple risk factors for glaucoma including: age, race, family history, corneal thickness, optic nerve size, history of eye trauma, steroid use, and high eye pressure to name a few. Treatment for glaucoma involves lowering the pressure in the eye, even when one’s eye pressure isn’t higher than normal. Lowering eye pressure is usually achieved using prescription eye drops, but some patients require surgical intervention to attain lower eye pressure to keep their glaucoma controlled. Although damage from glaucoma cannot be reversed, it can be slowed to try to preserve one’s vision throughout their lifetime. Annual comprehensive eye examination by our doctors is key to detect glaucoma early.
Dry Eye Syndrome
Occurs when there is a disruption in the normal cycle of one’s tear production. Dry Eye may be related to a “quality” or “quantity” issue or both. Some common symptoms of dry eye syndrome include: burning, tearing/watering, foreign body sensation, gritty/sandy feeling, redness, light sensitivity, fatigue and irritation. Risk factors for dry eye include: age, gender (female>male), environment (dry/poor air quality/UV exposure/wind), environmental allergies, computer use, medications, blepharitis/meibomitis, history of refractive surgery (LASIK/PRK) and systemic/inflammatory disease. In many cases, dry eye syndrome is a lifelong problem with symptoms that need to be “managed” but may not be able to be “cured” completely. Treatments for dry eye may include any of the following: over-the-counter artificial tears or gel, prescription topical dry eye drops, prescription oral anti-inflammatory medications, special eye vitamins, warm compresses with lid hygiene, and punctal plugs. Hydration, use of humidifiers, dry eye goggles, turning down fans in one’s environment are all other simple solutions to reduce symptoms related to dry eye. Talk to our doctors about your symptoms and if you have dry eye syndrome, what options may be best for you.
 Keratoconus
Keratoconus
Is a disorder that causes distortion of the cornea, the clear outer front covering of the eye. A normal cornea is gently curved, but in keratoconus the cornea becomes cone-shaped. This protruding of the cornea causes blur due to warping of light as it enters through the surface of the eye. Depending on the severity of the disease, the cornea may bulge and thin. When glasses are unable to correct the irregular astigmatism caused by the distortion, special contact lenses designed to vault over the bulge helps to create a more normal, smooth surface for light to pass through. This smoother surface helps to obtain a clearer image on the retina as light enters the eye. These contact lenses are typically either unique rigid gas permeable contacts or scleral lenses. Both require specialized expertise in achieving an optimal fit, for the best comfort and vision possible. Our doctors have extensive experience in fitting these specialty contact lenses. In some cases, a corneal transplant surgery may be a last resort to achieve better vision if other vision correction options are unsuccessful. Schedule an appointment today for us to determine how we can maximize your quality of vision while living with keratoconus.
Call us at 989-773-2020
for information on fees and scheduling
